9 July, 2024
Advances in Intestinal Rehabilitation: An exciting time to be a dietitian working in this field!
Parenteral Nutrition (PN) is a lifesaving intervention for those who need it. PN refers to the feeding of a person intravenously with a nutritional formula, specifically formulated for that person. As a clinical specialist dietitian working in intestinal failure (IF), many of the patients I look after are on PN at home.
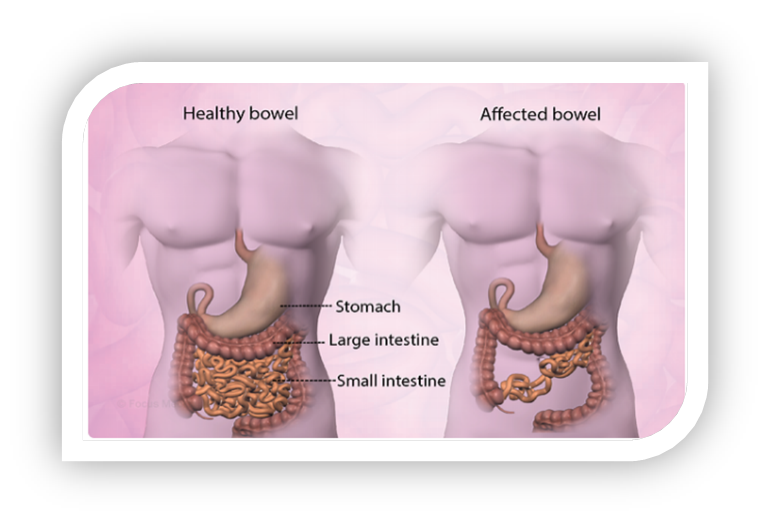
Intestinal failure is where there is an inability of the gut to absorb sufficient carbohydrates, protein, fat, vitamins, minerals and water therefore requiring intravenous supplementation to maintain health or facilitate growth. Depending on the disease indicating the need of PN, the duration of treatment can vary in length - some of our patients have been on PN since they were infants and others commenced on PN as adults. Short bowel syndrome (SBS), where the small intestine length is less than 200 cm, is the most frequent cause of IF.
| Parenteral Nutrition |
|---|
 |
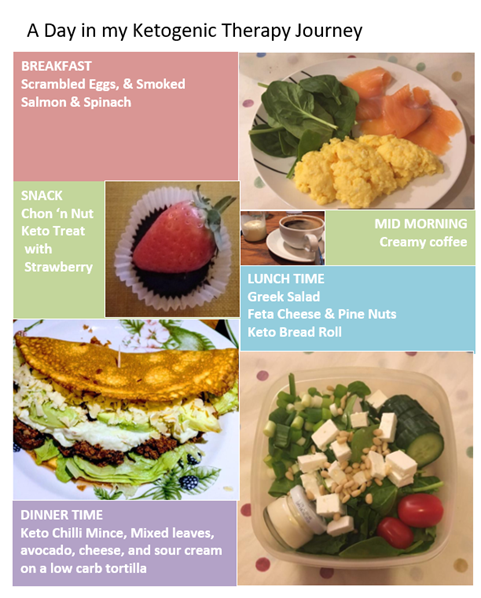
Managing Intestinal Failure patients on PN from a dietetic perspective is complex and time consuming. Every patient requires careful calculation of their nutritional requirements - including calories, protein, fat, fluid and vitamins and minerals. Overfeeding and giving too much fat or carbohydrate intravenously can damage the liver and contribute to potentially irreversible liver disease. Conversely, underfeeding patients leads to malnutrition and muscle loss. It is also a balancing act managing the vitamin and mineral content of the PN, too much of one could lead to toxicity and too little could lead to a deficiency, both of which can be dangerous. Excess of an electrolyte such as potassium, could result in cardiac arrhythmias. Each patient’s bespoke nutritional regimen is devised by taking into account their age, remaining bowel length and medical history, bloods, medications, weight and body mass index, as well as any diet or nutritional supplements taken. Nutritional management differs per goal and is tailored to the individual patient.
Although lifesaving, being on home PN is a massive burden and inevitably has an impact on the quality of life of patients. It is quite a time consuming intrusive procedure and the patients have to connect themselves for up to 12 hours a day, which imposes severe restrictions on daily life with regard to social and leisure activities as well as emotional wellbeing. PN also carries the risk of serious complications, including hepatic and renal dysfunction, and catheter-related bloodstream infections or thrombosis. Therefore, finding ways to improve the absorptive capacity of the remaining bowel and reduce PN is crucial to provide long-term well-being for those patients and this is referred to as Intestinal Rehabilitation. A new medication called Teduglutide provides such an option since 2021 in Ireland.

Teduglutide (Revestive®)
The active substance in Teduglutide is similar to human glucagon-like peptide 2 (GLP-2), a hormone made in the gut that increases absorption of nutrients from the intestine which ultimately reduces the number of days a week people with short bowel syndrome need parenteral support. The Consultant Gastroenterologist Dr. Cara Dunne is the only prescriber for adult patients in Ireland and the SJH Intestinal Failure team are now providing a national referral service for Teduglutide. There are currently six patients under the care of the team at SJH who have been commenced on Teduglutide. Some patients have been successfully weaned off PN completely or have been able to reduce parenteral nutrition. Others have recently started on Teduglutide with the aim is to wean their PN too.
To enable PN to be weaned on Teduglutide, it is imperative that daily oral fluid and caloric intake goals are met which requires intensive dietetic counseling and education in a cohort who have relied on PN to provide the majority of their nutritional input.
Working with Intestinal Failure patients is challenging, complex, but rewarding. I feel fortunate to be involved with pioneering Teduglutide nationally for short bowel syndrome patients on TPN, and it makes my dietetic role exciting and unique.