13 February, 2025
Happy International Epilepsy Day!
By Laura Healy, Clinical Specialist Dietitian in Ketogenic Therapy
A day to raise awareness and show support for those affected by epilepsy. Epilepsy affects everyone differently and there is no “one size fits all” approach to managing this condition.
Medical Ketogenic Therapy for Epilepsy: A Lifesaving Therapy
St James’s Hospital provides a National Ketogenic Therapy service, led by Dr Elisabeth Doran, for adults and patients transitioning from paediatric care. This treatment offers a powerful alternative for some adult patients whose epilepsy has not responded to other therapies.
In our experience, adult patients are often motivated to reduce anti-seizure medications (ASM) due to their side effects while aiming to improve seizure control. Not only does the ketogenic diet help control seizures, but it can also improve the overall quality of life for individuals with epilepsy. Fewer seizures mean fewer disruptions to daily activities, allowing individuals to engage in school, work, and social activities more easily. Secondary benefits include weight loss (if desired), improved mental health and of course, reduced risk of injury.

Dr. Elisabeth Doran and Dr. Laura Healy sharing their experience of Adult Ketogenic Therapy @KetoAdvance, London in 2024.
Effectiveness of ketogenic therapy in adults
Approx. half of adults can achieve greater than 50% reduction in seizures, as well as marked improvements in energy, alertness and wellbeing, even without changing ASMs. By the time ketogenic therapy is considered in medically refractory adults with epilepsy, often after multiple ASM and other treatments e.g. VNS have failed, so the true efficacy of ketogenic therapy may be underestimated.
What is involved in ketogenic therapy?
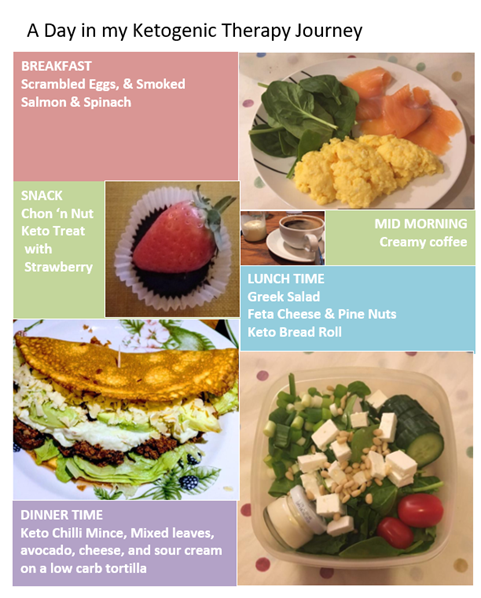
Ketogenic therapy involves a considerable change in food choices reducing carbohydrate intake and increasing healthy sources of fat. It is this reduction in carbohydrates (approx. 20g/day) that forces the metabolic shift to ketosis, where the body starts to burn fat for its energy instead of glucose. Ketones, which the body produces from fat, act as an alternative fuel source for the brain.
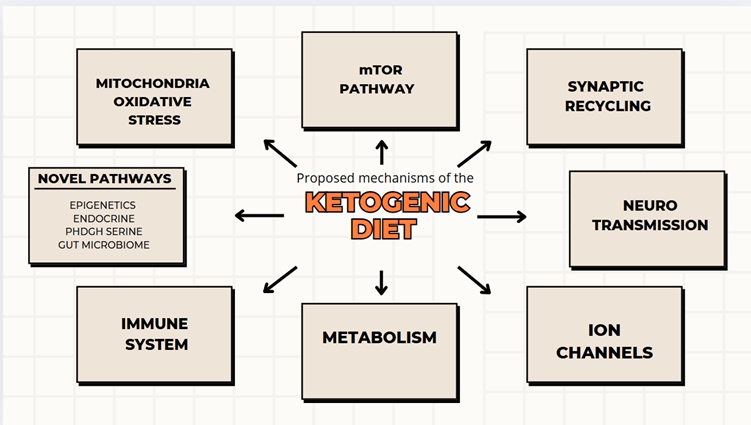
Ketogenic Therapy is Neuroprotective
The therapeutic mechanisms of ketogenic therapy are likely multifactorial and involve a complex range of metabolic changes. These changes affect neuronal activity in ways that may reduce seizures (See Fig 1. Ketones mean the brain becomes less reliant on glucose, this may have a calming effect on the brain’s neurons, reducing the likelihood of seizures through multiple mechanisms. Importantly, ketogenic therapy is thought to be neuroprotective, generating interest in its potential therapeutic role in other neurological conditions.
I decided to try the ketogenic diet, an opportunity for CPD with a difference that allowed me to better understand the challenges my patients face. This experience enhanced my knowledge, and improved my ability to prepare, support and problem-solve with my patients. Here are some key insights form that experience.
- Ketogenic therapy requires a 24/7 commitment to eat the right macronutrients to maintain ketosis. Any increase in carbohydrate (intentional or not) will impair ketosis. While ketone readings provide useful feedback, the impact on seizure activity and quality of life is equally important.
- Preparation is key. The initial weeks can be the hardest, but it becomes more familiar and manageable with time and proper planning.
- Ketogenic therapy has been used to treat epilepsy for over 100 years. It is important to differentiate the medical ketogenic diet from the ‘magazine lifestyle’ versions.
1
- Although the food is delicious, it's not convenient. Planning-ahead and being prepared makes all the difference.
- Most side-effects e.g. constipation, high cholesterol are easily managed with the support of an experienced ketogenic team.
- Integration of ketogenic therapy into the medical management of epilepsy by the Neurology team, is critical to its success. The gut brain connection is complex and bidirectional.
- Resilience and empathy are required in equal measure. The idea that you food choices give an opportunity to take some control over treatment can be very empowering.
Conclusion
Ketogenic therapy offers an effective, non-pharmacological treatment option for individuals with epilepsy, particularly for those who have not responded to traditional medications. By reducing seizures and improving quality of life, the ketogenic diet has become a valuable tool in epilepsy management. With careful monitoring and support, the ketogenic diet can provide significant benefits for those struggling with drug-resistant epilepsy.